In that moment of biting us, the parasite goes from the mosquito, with a temperature at 21°C to 24°C, to the human, at 37°C, and it gets switched on. It has been lying in wait in the salivary glands, and it suddenly arrives in our skin and gets switched on. We started to think how we could generate a whole parasite that looks like it is switched on. That is one of my active research projects. But the second question, which is related, is what the protein surface coat (the aspect of the parasite that the immune system sees) looks like when the parasite is being switched on. Maybe it looks different to the parasite that we have been researching for decades, which is isolated from the mosquito.
Jake Baum
Developing a malaria vaccine
Jake Baum, Head of School of Medical Sciences at UNSW, Sydney, explains the challenges of developing a full malaria vaccine.Key Points
- • Nearly half a million children die each year from malaria. A fully effective malaria vaccine will be the game changer. The two main malaria vaccines today offer only 30% to 40% protection from the disease.
- • The challenge we have is that malaria is an eukaryotic cell. It is a cell like one of ours. It is not a bacteria. It is not a virus. It has a nucleus. So, it has a complicated genome.
- • Testing safety, demonstrating protection and overcoming logistics are challenges of developing a successful malaria vaccine.
Malaria vaccine: the missing ingredient
For many years following my PhD, I was dedicated to studying the cell biology of the parasite that causes malaria, to understand how it works and how it moves. It is an ancient cell, and I thought that would be a fascinating project to sink my teeth into. For a number of years, mainly based on serendipity, we worked on drug screening and drug discovery.
But in the last five years, I have started to believe that the only way we are going to ever crack global malaria is through a new vaccine. We need many things to happen, but the key missing ingredient that we still do not have is a fully effective malaria vaccine: a vaccine that can be deployed to the developing world, where it can be used to readily immunise children, because nearly half a million children die each year from malaria. That will be the game changer. All the other pieces of the pie are still necessary. But for the next phase of my research career, I want to work on a vaccine against malaria.

What makes malaria different?
The challenge we have is that malaria is an eukaryotic cell. It is a cell like one of ours. It is not a bacteria. It is not a virus. It has a nucleus. So, it has a complicated genome. There are many clever aspects to its biology. Eukaryotic cells are detailed entities, living things, and nobody has ever made a vaccine that targets a human eukaryotic parasite or eukaryotic pathogen. Yes, there are vaccines against lots of viruses and bacteria, but nobody has made one against something as complicated as a malaria parasite cell. That is a major challenge.
What does it mean to work on a vaccine?
For me, it means trying to understand what works best and what does not work so well. The malaria field at the moment is dominated by two types of vaccine. The first type of vaccine is the parasite itself, but given in a way where the parasite is attenuated so it does not cause disease. The second strategy involves taking the key proteins that seem to immunologically define the parasite. That means taking the things that dominate its surface and turning those into a successful vaccine, a so-called subunit vaccine.
There are currently two vaccines that are at the forefront of malaria parasite vaccinology. They are both being trialled in the field in people, and both show about 30% to 40% efficacy. So, 30% to 40% protection against disease. It does not seem to last long. Maybe up to a year, maybe a bit more. That is disappointing as a vaccine. You might think that with all this time, all this research that has gone into a vaccine, maybe we should give up. But one option is to stand back and think: what are the things that have not changed?
Two new lines of research
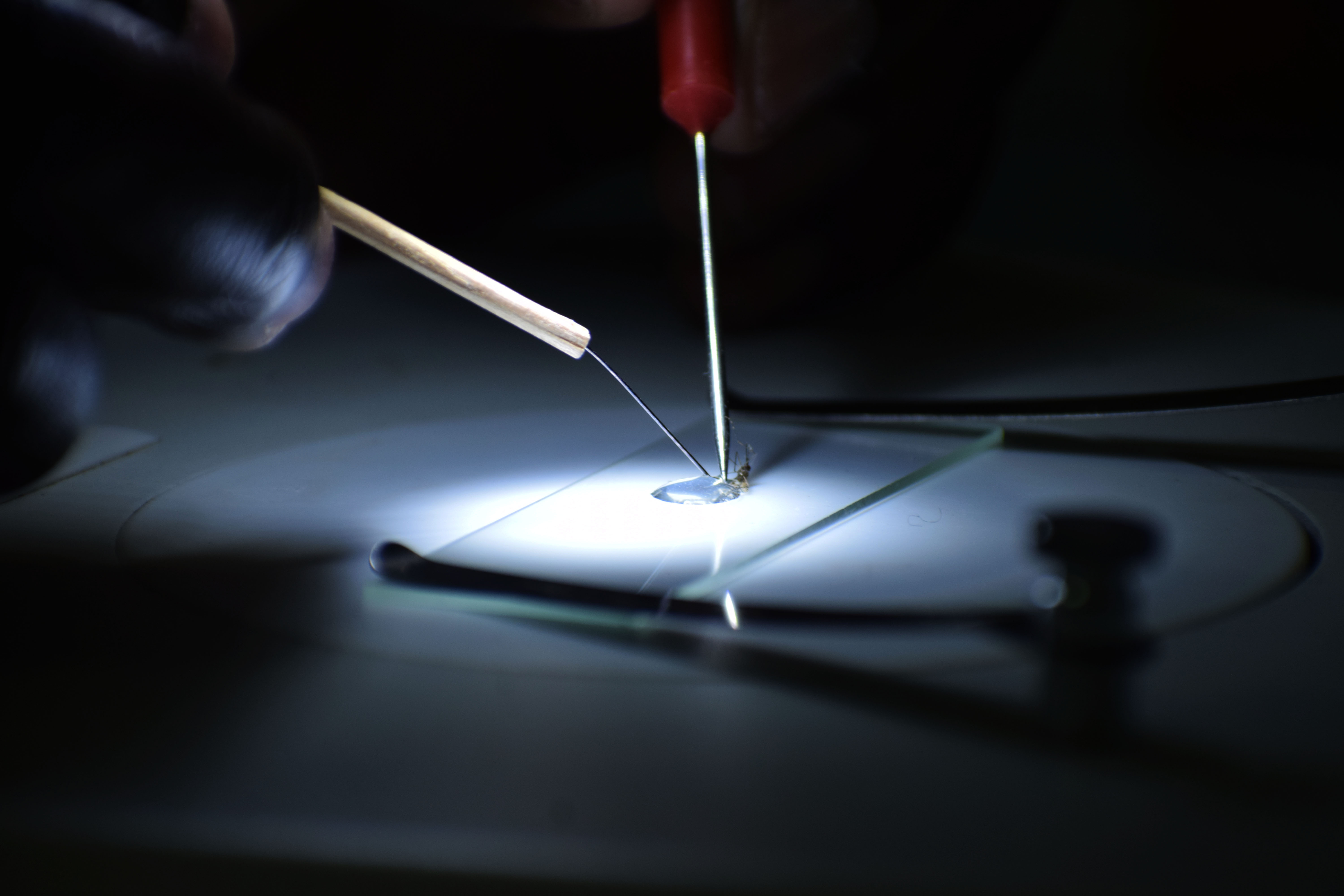
There are two things that we are passionate about. One is the parasite itself. The current vaccine that is based on the whole parasite is still removed from the mosquito, which infects you with malaria. It is removed from the mosquito by painstaking dissection: taking off the head and taking a parasite from their tiny banana-shaped salivary glands. Taking the parasite out is a laborious process. But that is not how we get infected with malaria. We do not get infected with malaria from the parasite, from the saliva gland. We get infected by malaria when the mosquito bites us.
Does the malaria parasite use a decoy?
One idea, which is slightly controversial, is about the main protein that the immune system sees. The protein that dominates the surface of this sporozoite comes from the mosquito’s salivary gland and enters our skin. The main protein of the sporozoite surface is called CSP, circumsporozoite protein. It is abundant on the surface. If you inject mice or humans or anything with malaria parasites, you get a huge immune response against CSP.
But maybe CSP is the decoy. Maybe CSP is the one molecule the parasites invented to get the immune system to recognise the wrong thing because it is so abundant; it is like a smokescreen. One of the ideas that we are pursuing is what lies under CSP. Maybe there is another protein under there. There is a famous vaccine that is the most advanced in clinical trials. It is called RTS,S and it is based on this protein, CSP, the protein that dominates the parasite’s surface. If that is the decoy or if there are elements of it that are a decoy, then maybe that would explain why the current vaccine strategies are not working so well.
Exploring different paths to a vaccine
There are two key strategies that we are pursuing, as we try and address this thorny question of the malaria vaccine.
One is addressing this molecule CSP. Maybe it is the perfect vaccine target and maybe our current usage of it is not in the perfect form. Or maybe there are other proteins that we have never looked at because we cannot see the wood for the trees; all we can see is this protein, CSP, but maybe under the surface there are other molecules that could make good vaccines.
Another is about trying to deliver this whole parasite in a way that mimics infection, where we know you can get protection, but boosting that potential. It can also be looking at the parasite protein chemistry, the proteins that are abundant on the surface, while giving the parasite some credit. It has had millions of years to evolve its biology. It has had tens of thousands of years to co-evolve with human populations. Maybe the main protein it puts out and the main protein we see is a decoy or a smokescreen, hiding the good stuff. If we could launch an immune response to that, it might be more effective.

From the lab to the clinic: the translation
As a researcher working on a global infectious disease, it is tempting in grants and papers to say: this might help make a malaria drug or this might help make a malaria vaccine. Actually, we would like to make a difference, to translate our understandings from the lab, from the bench, and bring them to something that might work as a malaria therapeutic or malaria vaccine. Anybody who works in or has even tasted that world of translation knows that it is a painstaking process to take an idea from the lab and translate it into something that might make it into the clinic.
Vaccines take time
One of the reasons why the vaccines and drugs that we all go to might still not work well is that it takes so long to get the next idea through the door and into the clinic. You need to go through all the stages. There is the actual idea itself. It has to be a good idea, robust, based on sound science.
You nearly always have to test your vaccine idea in some kind of preclinical model. The normal choice is the mouse. The mouse is well studied; we understand its immune system. It is not perfect, but a good predictor of what might happen in a human. Then we have to go through a series of detailed assessments to work out whether that thing that was potentially going to be put into somebody’s arm is safe and has no other side effects. Often, the first years of vaccine development are mostly about safety. Is this a safe thing to put into somebody’s bloodstream or into their skin, into their muscle? That is the safety process. But there are all these other processes as well.
Logistical challenges to developing a vaccine
For somebody working on malaria, you have to think that malaria predominantly affects children in Africa, and in rural Africa. There is a lot of breaking or non-existent infrastructure. That creates challenges for a cold chain: the idea that something could be frozen in a lab in Europe or North America, taken to the field still frozen and only thawed in that last minute. How do we preserve our vaccine for that journey? How do we deliver it so that it reaches the person who needs it in the most active form? And how do we formulate it?
The whole world of formulation are these things called adjuvants, things that are mixed with a vaccine to make the immune system see it and switch the immune system on. Adjuvant technologies are extremely complex, too. We have safety, formulation, preservation, delivery: all of those kinds of elements. That is all before we have even thought about a robust clinical trial. The early stages of vaccine development involve small-scale clinical trials.
How to test an experimental vaccine
To address this question of safety, you have to address this question of immunogenicity. If I give my experimental vaccine to somebody, do they make an immune response? But that is not evidence that it is going to work; the key thing you need is evidence of protection. With malaria, we are fortunate because we can give somebody malaria under control conditions, controlled human malaria infection (CHMI). We can give them the CHMI because we have a drug for the control parasite.
We give them a parasite that we know well. We have a drug that will cure them of malaria 100%. We can give them malaria, and we can cure them accurately. We have a platform where we can vaccinate somebody with an experimental vaccine or a placebo. We can give them malaria and then the vaccine plus malaria. Are they protected? With small numbers, you can progress a malaria vaccine to field in five to ten years. You can imagine getting a vaccine to clinical trial and potentially to the early stages of testing and in healthy adults. To say a decade or two decades is probably not an overestimate.
The journey to developing an effective vaccine
Now, we are living in a pandemic with a disease that we do not have a cure for. It is much harder to bring a vaccine to market. You have to be able to show that it is safe; you have to show that it is immunogenic. But you also have to be able to show that it is protective. If you cannot give people the infection under control conditions, to show that it is protective is very challenging.
Often, you have to find a population where there is a lot of that disease, give the vaccine, give the placebo and then hope that you find enough people – enough statistical power – to show that it is protective. The journey is about trying to walk the walk. We do not want to say our research is important for protection. We want to actually do it. We have to be willing to walk for a long time. And it is a laboured process to take your idea from bench to bedside. But it is a walk that we are excited to begin.
Discover more about
potential malaria drugs and vaccines
Saunders, C. N., Cota, E., Baum, J. et al. (2020). Peptide probes for Plasmodium falciparum MyoA tail interacting protein (MTIP): exploring the druggability of the malaria parasite motor complex. ACS Chemical Biology, 15(6), 1313–1320.
Warszawski, S., Dekel, E., Campeotto, I. et al. (2019). Design of a basigin-mimicking inhibitor targeting the malaria invasion protein RH5. Proteins: Structure, Function, Bioinformatics, 88(1), 187–195.
About Jake Baum
Here's how we use cookies
To give you the best experience, we tailor our site to show the most relevant content and bring helpful offers to you.
You can update your preferences at any time, at the bottom of any page. Learn more about how your data is used in our cookie policy.